Prostatitis is an inflammatory disease of the prostate gland. It is manifested through frequent campaigns in the toilet, penis pain, scrotum, rectum, sexual disorders (erection, early ejaculation, etc. ), sometimes delayed urine and blood insurance in urine. The diagnosis of prostatitis is found by a urologist or other specialist in a typical clinical picture, the results of a rectal examination. In addition, prostate ultrasound is performed, prostatic secretion and urine bacteria sow. Conservative treatment - antibacterial therapy, immunotherapy, prostate massage, lifestyle correction.
Prostatitis - inflammation of the seeds (prostate) gland - prostate. This is the most common disease of the genitator system in men. Most commonly affects patients aged 25-50 years. In accordance with various data, prostatitis suffers from 30-85% of men over 30 years of age. Perhaps abscess of the prostate gland, inflammation of the testes and appendages, which threatens infertility. Climbing the infection leads to inflammation of the upper parts of the genius system (cystitis, pyelonephritis).
The pathology develops when an infectious agent is introduced, which enters the tissue of the prostate from the organs of the genius system (urethra, bladder) or from a remote inflammatory focus (with pneumonia, influenza, tonsillitis, boils).
Gold Staphylococcus aureus (Enterococcus), Enterobacter (Enterobacter), Pseudomonas (Pseudomonas), Proteus (Proteus) and Klebcelllah and Klebcelllah can act as an infectious agent in the acute process. (Klebsiella) and E. Coli (E. Coli). Most microorganisms belong to the conditionally pathogenic flora and cause prostatitis only if there are other predisposing factors. Chronic inflammation is usually caused by Paul with microbial associations.
The risk of developing the disease increases during hypothermia, the presence of specific infections and conditions in the history of congestion in the tissues of the prostate. The following predisposing factors differ:
The risk of pathology is thought to increase with chronic intoxics (alcohol, nicotine, morphine). Some studies in the field of modern andrology have shown that the provocative factor is a chronic injury to the crotch (vibration, concussion) in motorists, motorcyclists and cyclists. However, the overwhelming number of experts believes that all the circumstances listed are not real causes of the disease, but contribute only to exacerbation of the latent inflammatory process in the tissues of the prostate.
The decisive role in the appearance of prostatitis is played by stagnation in the tissues of the prostate. Disruption of capillary blood flow leads to an increase in lipid peroxidation, edema, exudation of the tissues of the prostate and forms conditions for the development of the infectious process.

There are three stages of acute prostatitis that are characterized by the presence of a particular clinical picture and morphological changes:
In rare cases, chronic prostatitis becomes the result of an acute process, but as a rule a primary chronic course is observed. The temperature occasionally rises to small values. The patient notes mild pain in the perineum, discomfort during the act of urination and bowel movements. The most characteristic symptom is the scarce discharge from the urethra during the act of defecation. The main chronic form of the disease develops for a significant period of time. It is preceded by stagnation of blood in the capillaries, gradually becoming an abacus prostatitis.
Chronic prostatitis is often a complication of the inflammatory process caused by the causative agent of a specific infection (Chlamydia, ureaplasma, gonococcus). The symptoms of a specific inflammatory process in many cases mask the manifestations of the prostate lesion. It is possible to increase pain during urination, mild pain in the perineum, scarce discharge from the urethra during bowel movements. The slight change in the clinical picture often goes unnoticed by the patient.
Chronic inflammation of the prostate gland can be manifested by a burning sensation in the urethra and perineum, dysuria, sexual disorders, increased general fatigue. The consequence of potency disorders (or fear of these disorders) often becomes mental depression, anxiety and irritability. The clinical picture does not always include all these groups of symptoms, it differs in different patients and changes in time. There are three basic syndromes characteristic of chronic prostatitis: pain, disorders of toilet, sexual disorders.
There are no pain receptors in the prostate tissue. The cause of the pain in chronic prostatitis becomes almost inevitable due to the abundant innervation of the involvement of the pelvic organs in the inflammatory process of the nerve pathways. Patients complain of pain of varying intensity - from a weak, patient to intense, disrupting sleep. There is a change in the nature of pain (enhancement or weight loss) with ejaculation, excessive sexual activity, or sexual abstinence. The pain emits to scrotum, sacrum, crotch, sometimes in the lumbar region.

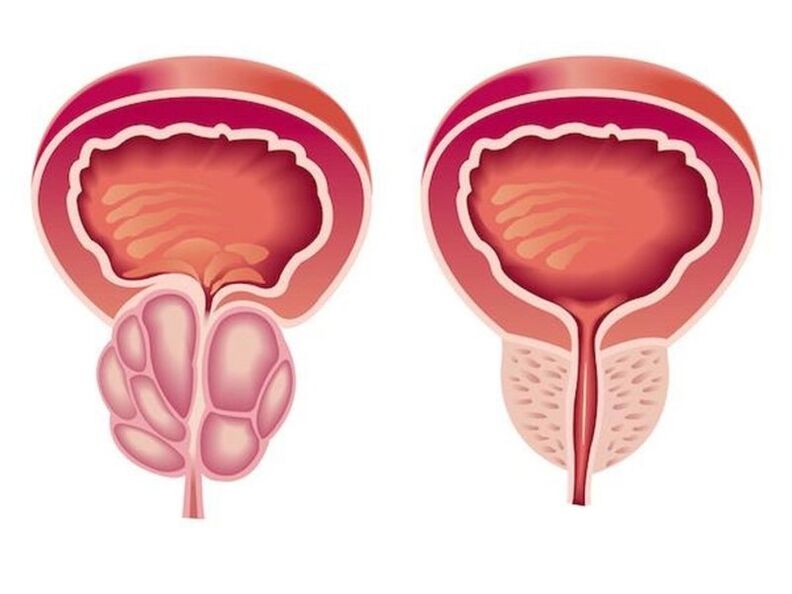
As a result of inflammation in chronic prostatitis, the volume of the prostate, which presses the urethra, increases. The lumen of the ureter decreases. The patient has frequent urination, a feeling of incomplete emptying of the bladder. As a rule, dysuric phenomena are expressed in the early stages. Thereafter, compensatory hypertrophy of the muscle layer of the bladder and urethra develops. Symptoms of dysuria during this period weaken and then increase again during decompensation of adaptive mechanisms.
In the initial stages, potency disorders may develop, which occur differently in different patients. Patients may complain of frequent night erections, deleted orgasm or worsening erection. Accelerated ejaculation is associated with a reduction in the level of excitation of the center, which is responsible for getting an orgasm. Ejaculation pain can cause sexual activity. In the future, sexual disorders become more pronounced. Impotence develops at an advanced stage.
The degree of sexual disorder is determined by many factors, including the sexual constitution and the psychological mood of the patient. Potential and dyisuria disorders can be due to both changes in the prostate gland and how easily a patient can inspire anything. If it has chronic prostatitis, it expects the inevitable development of sexual disorders and urinary disorders. Particularly often psychogenic disorders in the potency and problems with walking in the toilet develop in impressive, anxious patients.
In the absence of timely treatment of acute prostatitis, there is a significant risk of developing a prostate abscess. When a purulent focus is formed, the patient's body temperature rises to 39-40 ° C and may become fast-paced. The heat periods alternate with pronounced chills. Acute pain in the perineum complicates urination and makes defecation impossible.
The growth of swelling of the edema leads to a sharp slowdown in urination. In rare cases, the abscess spontaneously opens in the urethra or rectum. When opening in the urethra, a purulent mud urine with an unpleasant pungent odor appears when it opens in the rectum, the stool contains pus and mucus.
Chronic prostatitis is characterized by a wool -like course, with periods of prolonged remissions, during which inflammation in the prostate occurs latent or manifests itself in extremely scarce symptoms. Patients who are not worried often stop treatment and are converted only with the development of complications.
The most frequent complication of the chronic process is the inflammation of the testes and appendages of the testes and inflammation of the seed bubbles. The result of these diseases is often infertility.

A characteristic clinical picture simplifies the process of diagnosis in acute and chronic prostatitis. Required:
Patients with an acute process without complication undergo a course of treatment with an outpatient urologist. Hardly intoxication indicates suspicion of a purulent process, hospitalization. Antibacterial therapy is performed. Medicines are selected taking into account the sensitivity of an infectious agent. Antibiotics are widely used that can penetrate well into prostate tissue (ciprofloxacin, etc. ).
With the development of acute slowdown in urination, against the background of prostatitis, they resort to the installation of a special tube rather than a urethral catheter, as there is a risk of prostate abscess formation. With the development of an abscess, endoscopic tractal or urethral opening of the abscess is performed.
Treatment for chronic prostatitis should be complex, including etiotropic therapy, physiotherapy, immunity correction:
Chronic, long -term inflammation indicates a consultation with an immunologist to choose the tactics of immunocorogative therapy. The patient receives recommendations for lifestyle change. The introduction of certain changes in the lifestyle of a patient with chronic prostatitis is both therapeutic and preventive measure. The patient is advised to normalize sleep and alertness, to establish a diet and to have moderate physical activity.

Acute prostatitis is a disease that has a pronounced tendency to chronic. Even with timely adequate treatment, more than half of patients, chronic prostatitis becomes the result. Recovery is far from always possible, but with proper consistent therapy and adherence to the doctor's recommendations, it is possible to eliminate unpleasant symptoms and to achieve a long constant remission in the chronic process.
Prevention consists in eliminating risk factors. It is necessary to avoid hypothermia, alternative stuck work and with periods of physical activity and to eat regularly and completely. Constipation should be used laxatives. One preventative measures is to normalize sex life, since both excessive sexual activity and sexual abstinence are risk factors for the development of prostatitis. If the symptoms of urological or sexually transmitted disease occur, you should consult a doctor in a timely manner.
























